BASL 2025 comes to Belfast


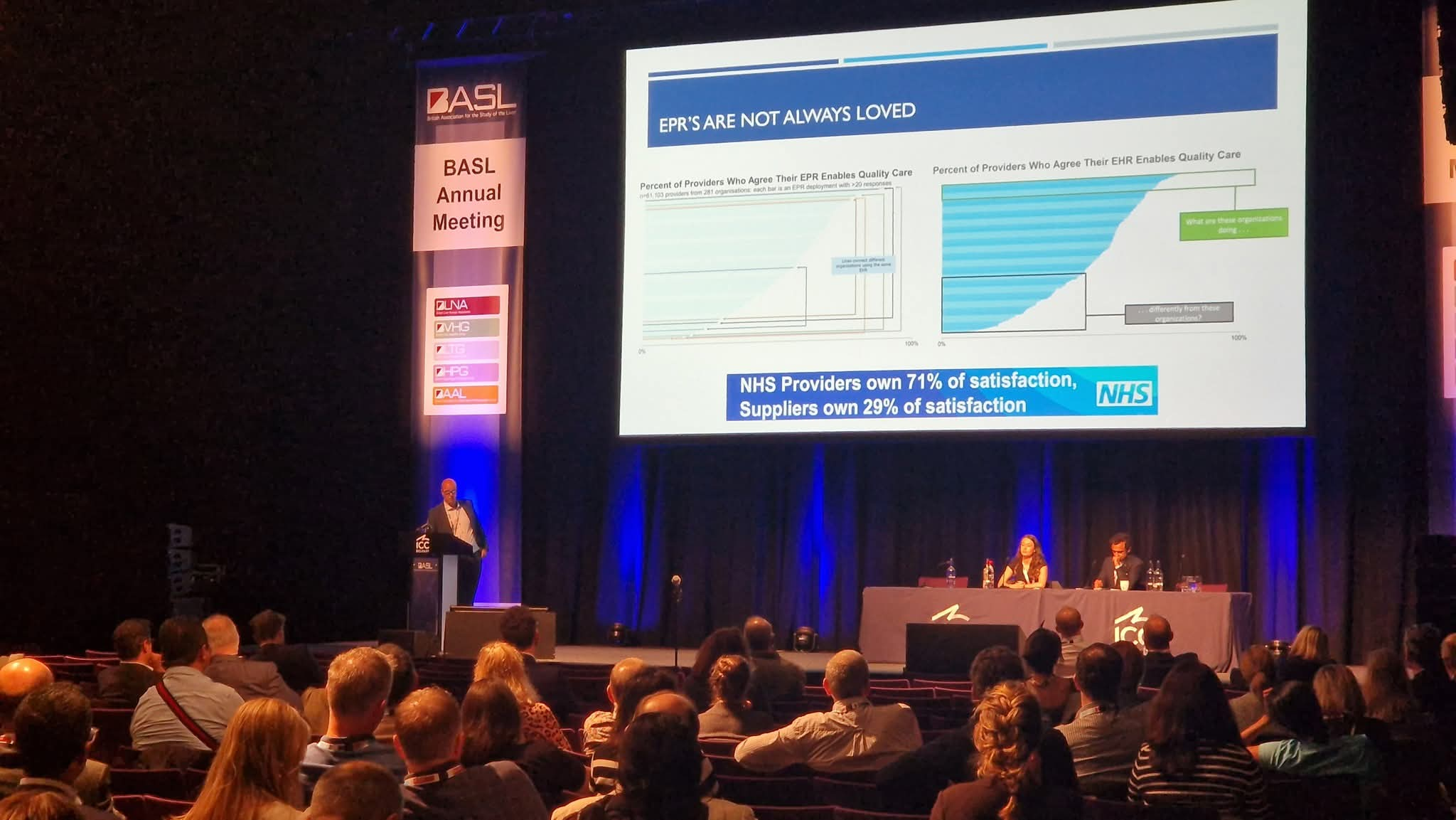

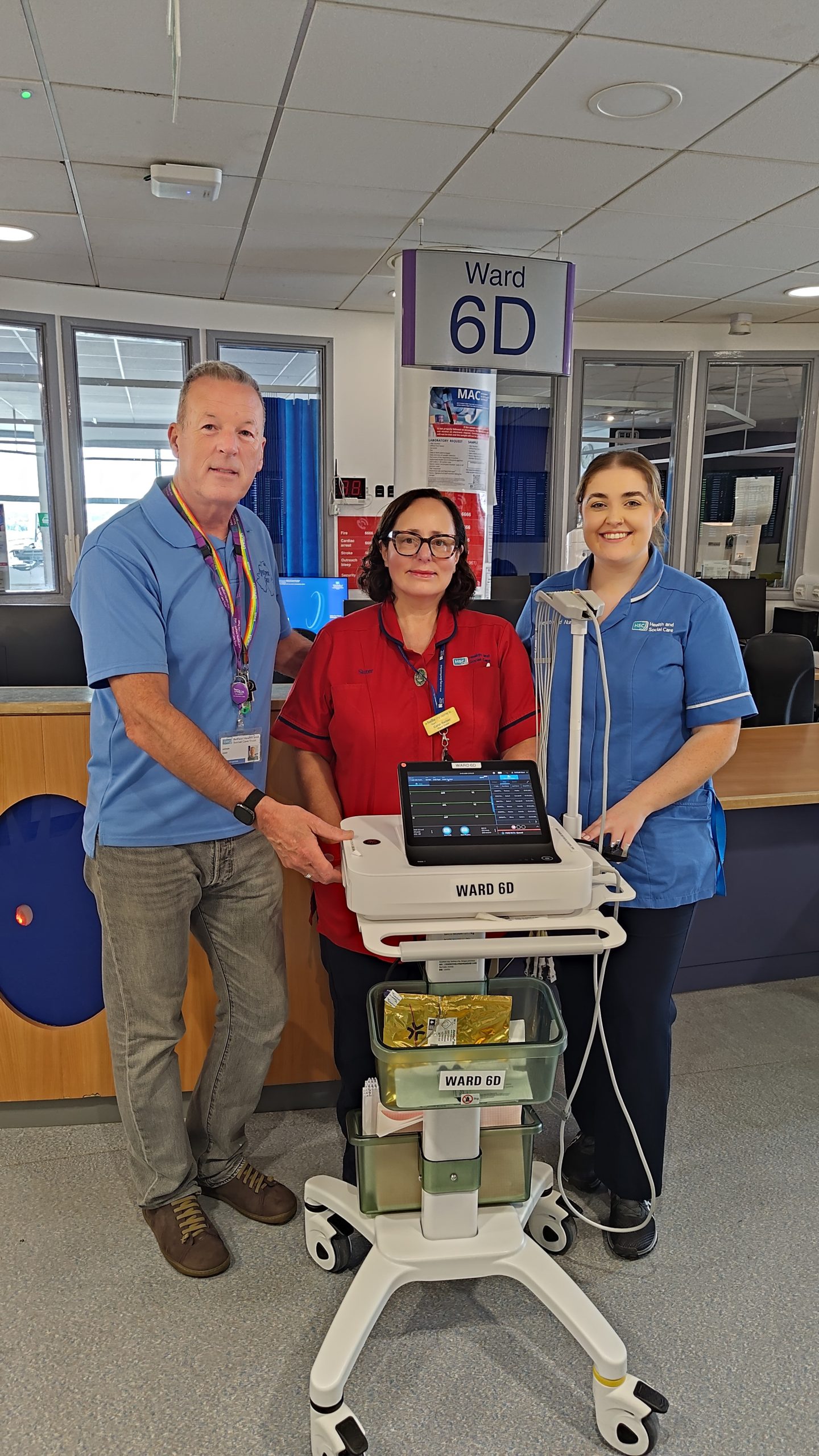
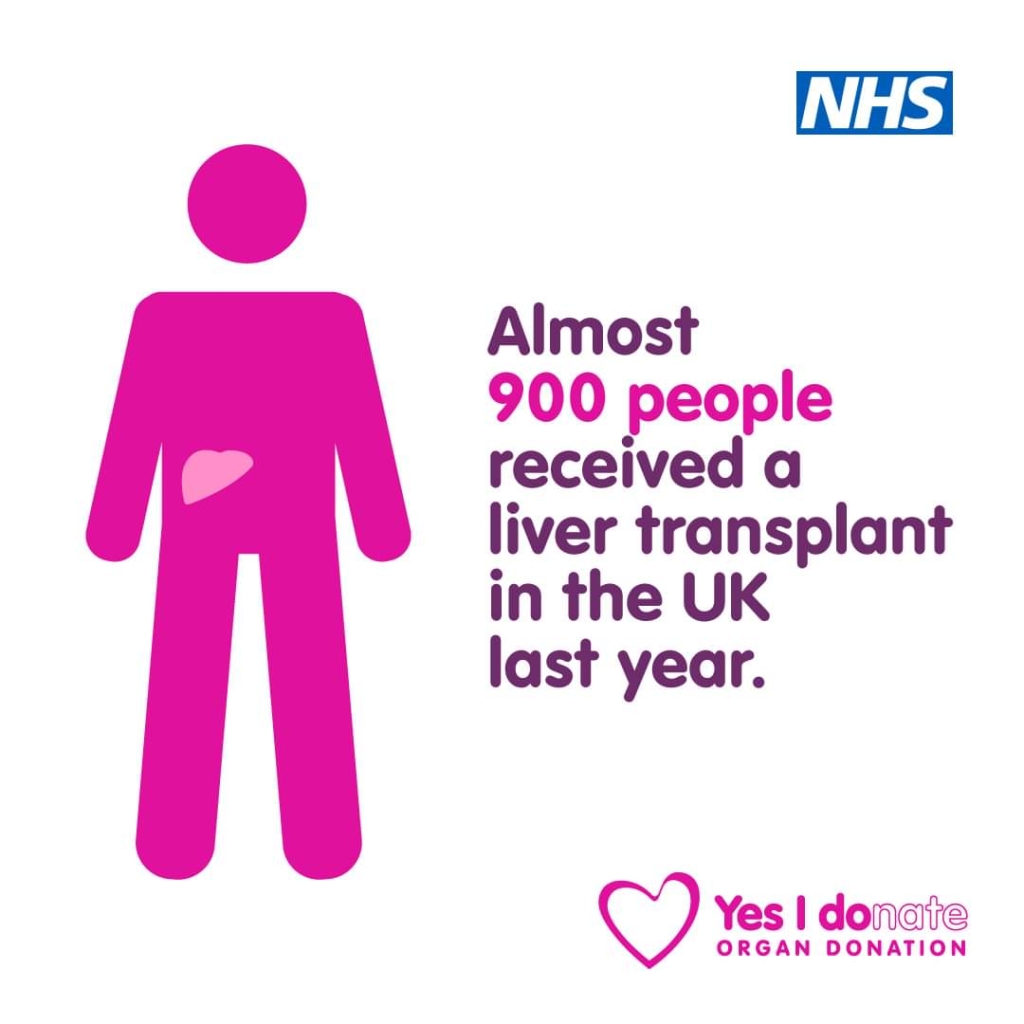
This week we attended BASL 2025, a liver conference at the ICC, Waterfront Belfast. What is BASL I hear you ask. Well, it stands for the British Association for the Study of the Liver! This is the first time that it has been held in Belfast and , as a charity associated with the liver, we were proud to be in attendance at the event.
Medical staff from all over the UK attend this conference each year where everyone is kept up to date on all of the recent medical research, interventions and treatment therapies.
During the course of the week we met liver professionals from all over the UK and Ireland and informed them of what we do for all liver patients in N Ireland.
We would like to thank our consultants and all of the staff from the Province’s hospitals who came visit us at our table.